Abstract

Background: Tabelecleucel is an investigational, off-the-shelf, allogeneic Epstein-Barr virus (EBV)-specific T-cell immunotherapy being studied in patients (pts) with serious EBV-driven diseases, including post-transplant lymphoproliferative disease (EBV + PTLD). The median overall survival (OS) after treatment failure of rituximab is short at ~1.7 months in EBV + PTLD following hematopoietic cell transplant (HCT) (Socié EBMT 2020) and ~3 months in solid organ transplant (SOT) recipients with EBV + PTLD whose disease relapsed after rituximab and who did not respond to or did not receive chemotherapy (CT) (Zimmerman EHA 2019). These poor outcomes demonstrate an urgent unmet need for effective therapies in this ultra-rare serious disease. Promising outcomes have previously been demonstrated (Prockop JCI 2020). Additionally, we have shown clinical benefit with a >60% objective response rate (ORR) and >80% estimated 2-year OS rates (Prockop EBMT 2021, Prockop ATC 2021) in pts with EBV + PTLD, irrespective of pts achieving a complete response (CR) or partial response (PR) to tabelecleucel. Safety data have been assessed in >150 pts with EBV + PTLD treated with tabelecleucel with tumor flare reaction (TFR) as the only identified risk. Here, for the first time, we report interim efficacy and safety results from the pivotal phase 3 clinical trial ALLELE (NCT03394365) - a multicenter, open-label study of tabelecleucel after failure of rituximab ± CT in pts with EBV + PTLD following SOT or HCT.
Methods: ALLELE is evaluating the clinical benefit of tabelecleucel in two cohorts: (1) pts with EBV + PTLD following SOT after failure of rituximab ± CT (n=33), and (2) pts with EBV + PTLD following HCT after failure of rituximab monotherapy (n=33). Tabelecleucel is administered at a dose of 2 x 10 6 cells/kg on days 1, 8, and 15, followed by observation through each cycle lasting 35 days. Response per clinical and radiographic assessment (by PET/CT) is evaluated by the investigator and by independent review using Lugano Classification with LYRIC modification. Key efficacy endpoints include ORR, duration of response (DOR), time to response (TTR), and OS. After treatment is completed or discontinued, pts are assessed every 3 months up to 24 months, and every 6 months thereafter for survival status up to 5 years.
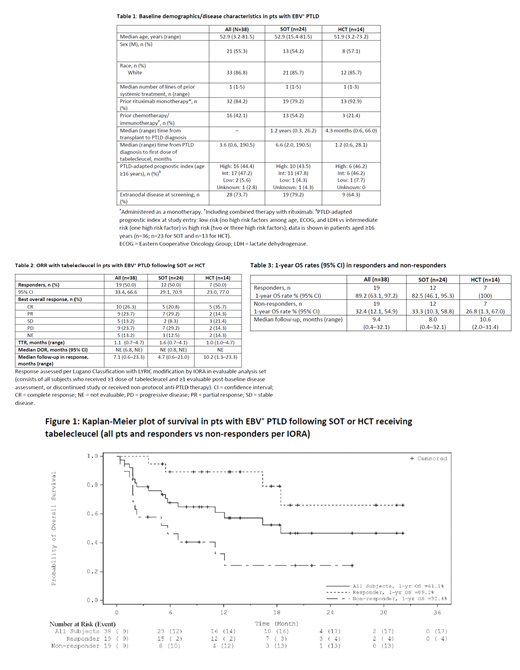
Results: As of May 2021, 38 pts (24 SOT, 14 HCT) were evaluable for response assessment by independent oncologic response adjudication (IORA) and had the opportunity for 6 months follow-up (Table 1). SOT and HCT pts received a median (range) of 2.0 (1-6) and 3.0 (1-5) cycles of tabelecleucel, respectively. ORR was 50% (19/38, 95% CI: 33.4, 66.6) in the overall population, 50.0% (12/24, 95% CI: 29.1, 70.9) in SOT, and 50.0% (7/14, 95% CI: 23.0, 77.0) in HCT, with a best overall response of CR (n=5, SOT; n=5, HCT) or PR (n=7, SOT; n=2, HCT; Table 2). Overall, median TTR was 1.1 months (0.7-4.7), 11 of 19 responders had a DOR lasting >6 months, and median DOR was not reached (Table 2).
Median OS was 18.4 (95% CI: 6.9, NE) months overall, 16.4 (95% CI: 3.5, NE) months for SOT, and not yet reached for HCT. 1-year survival rate was 61.1% (95% CI: 42.9, 75.0) overall, 57.4% (95% CI: 35.2, 74.5) for SOT, and 66.8% (95% CI: 32.4, 86.6) for HCT. Those who responded had a longer survival compared to the non-responders, with a median OS of NE (95% CI: 16.4, NE) and 1-year survival rate of 89.2% (95% CI: 63.1, 97.2). Non-responders had a median OS of 5.7 (95% CI: 1.8, 12.1) months and 1-year survival rate of 32.4% (95% CI: 12.1, 54.9) (Table 3).
Serious treatment emergent AEs (TEAEs) were reported in 62.5% of SOT and 57.1% of HCT pts. Fatal TEAEs were reported in 16.7% of SOT and 7.1% of HCT pts; none of the fatal TEAEs were related to study treatment. Tabelecleucel was well-tolerated with no reports of TFR and no confirmed evidence for graft vs host disease, organ rejection, infusion reactions, or cytokine release syndrome in relation to tabelecleucel in these treatment refractory and immunocompromised pts.
Conclusions: Tabelecleucel phase 3 interim data are reported here for the first time and show clinically meaningful outcomes and promising ORR and OS in a pt population with no approved treatment options and otherwise poor survival. Tabelecleucel, an allogeneic cell therapy, was well tolerated without evidence of safety concerns typically observed with autologous chimeric antigen receptor cell therapies.
Prockop: Memorial Sloan Kettering Cancer Center: Other: S Prockop receives support for the conduct of sponsored clinical trials through MSK from Atara Biotherapeutics, Jasper and AlloVir. , Patents & Royalties: S Prockop is a co-inventor on intellectual property (IP) licensed to Atara. S Prockop has waived rights to this IP to MSK and has no personal financial interests in Atara. MSK has financial interests in Atara and IP interests relevant to this abstract. ; Atara Biotherapeutics: Other: support for the conduct of sponsored trials and Inventor; Jasper: Other: support for the conduct of sponsored trials; AlloVir: Other: support for the conduct of sponsored trials; Neovii: Consultancy; ADMA Biologics: Consultancy; MSK: Other: Inventor. Mahadeo: Atara Biotherapeutics: Consultancy. Beitinjaneh: Kite/Gilead: Other: Ad Board Event Attendee. Choquet: Sanofi, Celegene, Roche, Abbvie, Sandoz, Janssen, Takeda: Consultancy. Stiff: Cellectar: Research Funding; CRISPR: Consultancy; Gamida-Cell, Atara, Amgen, Incyte, Takeda, Macrogenetics, Eisai: Research Funding. Reshef: Bayer, BMS, Regeneron, TScan, Synthekine, Atara, Jasper: Consultancy. Dahiya: Kite, a Gilead Company: Consultancy; Miltenyi Biotech: Research Funding; Atara Biotherapeutics: Consultancy; Jazz Pharmaceuticals: Research Funding; BMS: Consultancy. Parmar: Atara Biotherapeutics: Current Employment. Ye: Atara Biotherapeutics: Current Employment. Gamelin: Atara Biotherapeutics: Current Employment. Dinavahi: Atara Biotherapeutics: Current Employment.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal